
Crunch time: Putting the finishing touches on the 10 Year Health Plan
- Hospital waiting lists
- Health inequalities
- Lived experience
- Person-centred care
- Integrated care
- Primary care
As many of you will know, the Government is currently putting the finishing touches to its 10 Year Plan for the NHS.
This process involves bringing together all the insights they have received from the 270,000 people and organisations that have fed into the engagement process, combining it with the early work undertaken by the vision and enabler working groups, and working with policy teams within DHSC and NHS England to flesh out the detail.No easy task!
Those who have followed recent press coverage will know the pressure is now on to turn this in to a “retail offer”, to use the language of the Secretary of State, that patients will really notice and which will help rebuild public confidence in the NHS.
So, with crunch time approaching, we thought we would set out the five things National Voices will be looking out for in the final version:
Health inequalities
Tackling health inequalities has been a big feature of recent NHS strategies. The Elective Reform Plan for example set out a clear requirement for Integrated Care Boards (ICBs) to each produce a vision for how they will address inequalities in their respective backlogs including strengthening accountability of providers, improving the quality of demographic data to better track disparities, and providing very practical support with things like patient transport.
If the 10 Year Plan is to create a “retail offer” on inequalities, then it will need to continue this shift and implement specific and measurable policies that will make care more equitable. This could include the growth of initiatives already trailed, like the Community Health Workers, and deliberate moves to put new services like diagnostic hubs in areas affected by greater deprivation. We have also called for very practical improvements, like reviewing and expanding the NHS low income scheme.
Patient power
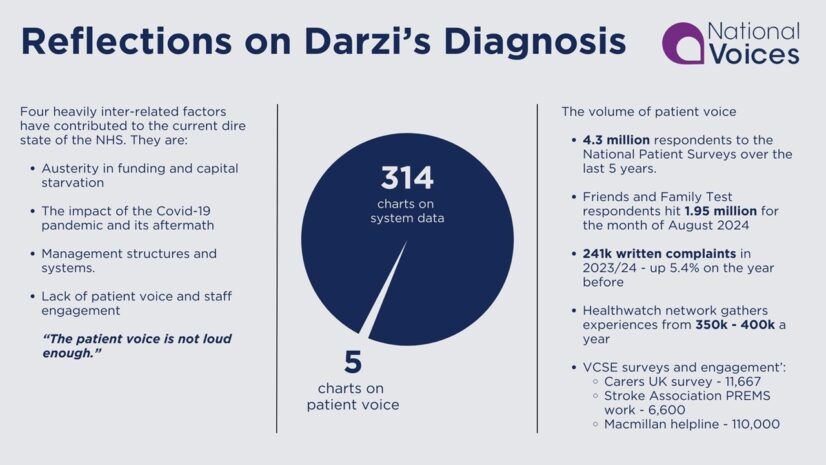
Lord Darzi’s review last summer concluded that the voice of patients isn’t loud enough. National Voices evidence argued slightly differently, that it’s not the volume of feedback from people and communities that is the problem, but a failure to listen and take action.
There has been much talk during the development of the 10 Year Plan about how it will increase the agency of individual patients, with more choice, more shared decision making and a greater emphasis on supported self-management, which we called for in our diagnosis report last year. But we also want to see a clear role for the collective voice of patients, including an enhanced role for patient feedback and a clear role for people with lived experience to contribute to policy development, and to be embedded into decision-making structures.
Measuring success
We know the Prime Minister has already made reducing the elective backlog, and getting back to the 18-week standard, a key performance indicator for Government as a whole. And the political reality is that we should probably expect the 10 Year Plan to continue with similar commitments around all the current constitutional standards.
But we would also like to see a longer-term move signalled by the plan, that in the future success of the NHS will be based on the outcomes it achieves, not just its outputs and number of activities. Take long term conditions (LTCs) for example, in a new National Voices’ report, due out later this month, we will argue how measuring patient experience and outcomes of the 25 million people with an LTC would be a more effective way of understanding whether or not the Government’s three shifts (to digital, community, prevention) are working.
The role of the VCSE
The announcement in March 2025 to abolish NHS England within the next two years and reduce ICB running costs by December 2025 have caused much concern among the VCSE, as we highlighted in our evidence to the Health and Social Care Select Committee. These reforms come on top of an incredibly tight financial climate which has already seen VCSE contracts and commissions cancelled or delayed indefinitely.
Yet it is also clear the NHS will not be able to achieve the shifts to prevention or community care, without our sector’s help. The 10 Year Plan needs to set a clear direction on partnership with the VCSE. This must be one where we are not just seen as a cheaper way to deliver services, but one that recognises the huge added value we bring. Given the timing in relation to the wider Government work on the Civil Society Covenant, there is big expectation on the Plan to set a more constructive partnership over the years ahead.
Deliverability
Lastly, but by no means least, people need to believe the plan can be delivered. This is more important than ever in light of the significant restructure the health service is now undergoing, and the complex legislative changes this may bring with it.
There may have been unprecedented extenuating circumstances for why the 2019 Long Term Plan wasn’t delivered in full, but we have seen plans before that also too often fell short. With public confidence being where it is on the NHS, we need a plan that is tangible and with a clear trajectory of how and when patients and staff will feel these improvements.
This is where “getting the basics right” comes in. This was a key message in National Voices pre-election manifesto, and we have seen the same sentiment come through strongly in the DHSC’s public engagement exercise. So, the Plan needs to be optimistic, but also realistic in what it can achieve. There will undoubtedly be huge technological advancements in genomics, medicines and the use of AI over the next decade, but if the plan doesn’t fix basic problems, like people getting appointment notifications after the appointment has taken place, then it is unlikely to turn public confidence around in time.